
Aesthetic Dentistry Magazine
By Christian Yaste, DDS
If you asked physicians to name one of the most common afflictions from which Americans suffer, chances are they will say “headaches.”
Chronic headaches are an overwhelming problem in the United States, with an average of 40 percent of Americans reporting chronic headache pain on a daily basis.1,2 While many people (in the general public and among the healthcare community) have traditionally assigned headaches and their respective care to the purview of physicians and specialists, it is becoming increasingly clear that dentists have a greater part to play in providing comprehensive pain relief.
According to the National Headache Foundation, approximately 90 percent of the U.S. population has headaches, and more than 37 million people suffer from migraines.3,4 Many of these patients have been suffering for years, seeking the advice of multiple healthcare professionals, trying any number of prescriptions or alternative medicines to find some relief, but often without success. Few, however, think to consult with their dentists.
Yet those in dentistry may have a good solution for many suffering Americans. An underlying condition causing many of these headaches and other pain symptoms is dentomandibular sensorimotor dysfunction (DMSMD), a condition involving imbalanced dental forces that dentists are uniquely positioned to treat.5 By expanding the scope of care to include treatment of this type of chronic pain, dentists can improve the overall quality of life for their patients. Simultaneously, dental practitioners will differentiate themselves from other practitioners and establish themselves as effective providers of care, adding immeasurable value to their practices.
How DMSMD Affects Patients
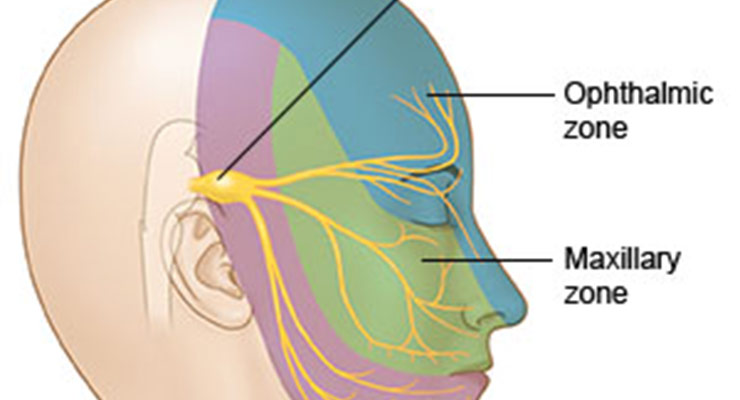
DMSMD generally presents in the form of headaches or migraines, but patients may experience numerous other symptoms. Such symptoms include tinnitus, myofascial pain, TMJ disorders, and changes in the brain’s neurotransmitter chemistry and balance. Additionally, many patients also present with multiple oral symptoms: bruxism, clenching, tooth wear, fracture or breakage, abfractions, and/or an unstable dental arch form. Other factors, such as malocclusion, may play a role, especially if clenching or bruxism is present.6 Since DMSMD results from improperly functioning dental forces, muscles may become unbalanced or overloaded, causing or perpetuating localized and referred pain impulses throughout the trigeminal cervical nucleus.7,8
In recent years, assessment technologies and sports-derived rehabilitative devices have demonstrated a clearer picture of the relationship that exists among dental forces, disease and dysfunction—all involving the oral environment and surrounding muscle tissue and nerves.9 Such advances have paved the way for an in-office system of care that is revolutionizing the way dentists are treating patients for a variety of DMSMD-related concerns. An Effective System
The TruDenta® system incorporates several comprehensive assessments to determine how patients can best benefit from the customizable treatments available. The treatments include range of motion (ROM) and bite force analyses to understand the effects that DMSMD is currently having on the patient’s well being. Additionally, patients are given a complete head health history form and comprehensive exam to establish parameters for treatment modalities. This detailed history gives patients an opportunity to clearly identify their pain and express any concerns they may have to the dentist. It also covers dental history and explores potential causes of their pain.
During the initial assessment, dentists use the TruDenta® system to provide patients with computerized measurements of the force balances in a patient’s mouth, on a tooth-by-tooth basis. Patients can also see an exact measurement of the disability of their facial and jaw muscles to determine where the imbalances are occurring. They receive a computerized analysis of their mouth movements to determine any additional bite force imbalances.
Dentists can then prescribe one of four levels of care, depending on the severity of the case. Based on the assessment, treatment plans may last between one and 12 weeks. The system itself provides clinicians with objective information to present to patients, so patients can understand why the symptoms have manifested. The digital system provides a detailed visual aid that proves immensely helpful to dentists in garnering patient acceptance of proposed treatment plans. This, in turn, means a greater success rate for the practice, with loyal patients who return for the full course of treatment.
Upon completion of treatment, pain is no longer an issue for patients, which means that restorative or elective dental treatments may be completed more easily and at a pace that is more comfortable to patients and dental teams.10 Thus, the system of care proves integral not only for eliminating the source of chronic pain for patients, but also for helping them on the path to better oral health.
Customized Treatment Modalities
Once patients have completed the necessary assessments to determine the appropriate level and length of care, dental teams provide a series of rehabilitation treatments designed to address the underlying causes of the patients’ imbalanced force-related problems and resulting pain symptoms. The TruDenta® system is designed to be non-invasive — thus highly conservative — with no drugs or needles involved. Patients undergo a unique combination of multiple therapies, both in-office and at home. Each in-office treatment is approximately 50 minutes and can include any of the following:
Manual Muscle and Trigger Point Therapy
This treatment modality targets facial and jaw muscles, identifying any trigger points that may have developed as a result of unbalanced dental forces. Found within bands of muscles, trigger points are often a source of pain and inflammation for patients. This therapy breaks up any trigger points or muscle knots, thereby increasing blood flow to the area, which simultaneously decreases inflammation and pain while promoting faster healing. This therapy alone can reduce patients’ need for pharmaceuticals and invasive dental procedures such as surgery.
Therapeutic Ultrasound
Designed to promote increased speed of healing, this method helps return circulation to muscles that have become sore or strained with improper use. It increases blood flow to the area, and the heat applied during the process reduces inflammation. Additionally, the sound waves work to break up scar tissue or deep adhesions that may have formed, perhaps as a result of injury or other trauma.
Transcutaneous Electrical Stimulation
This therapy is designed to reduce any muscle spasms and/or referred pain that patients may be experiencing. A low level electrical signal is used but its strength is sufficient to encourage nerve stimulation and decrease any lactic acid that may have accumulated over time. This therapy can also work to increase mouth opening in patients whose range has been decreased due to pain or inflammation.
Low Level Laser/Light Therapy
Like other treatments, this modality works to decrease pain and inflammation. However, it also reconnects the pathways of nerves to the brain stem, allowing muscle and joint tissue to heal faster as pain is inhibited. This therapy is especially useful for patients suffering from TMD symptoms, because the combination of the low-level laser therapy and electrical stimulation permits the patient’s musculoskeletal system to heal naturally, albeit at a much quicker rate. For patients experiencing painful TMD symptoms, this therapy can increase stability of the TMJ and increase the mouth opening.
Depending on the needs of patients and the severity of their cases, they may also be provided with a homecare kit to use after in-office treatments for further rehabilitation. Patients may also be fitted for a rehabilitation splint (to be worn temporarily, as directed) to retrain and balance muscles.
Opportunities for Dentists
Patients experiencing frequent headaches and chronic pain often search for answers as to why they are experiencing this type of pain and how they can resolve their issues. The exceptional capabilities of the TruDenta® system serves as the solution many patients are seeking, and clinicians should take advantage of this opportunity to expand their offerings. By adding the TruDenta® system to their services, dentists can separately brand a part of their practice to cater specifically to such patients, increasing revenue from patients who require this type of treatment, as well as any subsequent restorative treatments that require a stable foundation. These services can also be marketed to current dental patients that team members believe will benefit from this type of customized therapy.
As patients continue to search for a solution to the problems of headaches and chronic pain, dentists can position themselves as knowledgeable experts who can provide pain relief. Doing so benefits clinicians and patients alike. Patients experience the conservative treatment results a system like TruDenta® can bring, and dentists secure themselves a unique position as the providers of care that such patients so desperately need. The result is an increasing patient base and additional, incalculable value to their practices.
Endnotes
- Dawson P., Functional Occlusion: from TMJ to Smile Design. Canada: Mosby, Inc.; 2007.
- Hess LA., “The Relevance of Occlusion in the Golden Age of Esthetics.” Inside Dent. 2008;38-44.
- “How Donations Help,” National Headache Foundation, accessed May 1, 2014.
http://www.headaches.org/NHF_Store/Donations/How_Donations_Help - “How do you know if you have a migraine?” National Headache Foundation, accessed May 1, 2014.
http://www.headaches.org/blog/how-do-you-know-if-you-have-migraine - American Academy of Craniofacial Pain (AACP) Resources-For Patients. Headaches and Dental Health, accessed January 11, 2013.
http://www.aacfp.org/resources/headaches.cfm - U.S. News Health. Headache, Migraine, Tension Headaches, Cluster Headaches, accessed January 18, 2013.
http://health.usnews.com/health-conditions/brain-health/headache - Health Central. Migraine Presenteeism Creates More Lost Work Time, accessed on April 4, 2013.
http://www.healthcentral.com/migraine/understanding-migraine-404690-5_2.html - Jensen MP, Turner, JA, Romano JM, Karoly P., “Coping with Chronic Pain: A Critical Review of Literature.” Pain. 1991;47(3):249-283.
- Sessle BJ., “Mechanisms of Oral Somatosensory and Motor Functions and their Clinical Correlates.” J Oral Rehab. 2006;33:243-261.
- Locker D, Miller Y., “Evaluation of Subjective Oral Health Status Indicators.” Journal of Public Health. Dentistry. University of Toronto.
http://www.onlinelibrary.wiley.com/doi/10.1111/j.1752-7325.1994.tb01209.x/abstract





 © 2026 - NATIONAL DENTAL SYSTEMS, INC. | 430 NORTH MAIN ST. SALEM, UT 84653 | CALL US TOLL-FREE 855-770-4002
© 2026 - NATIONAL DENTAL SYSTEMS, INC. | 430 NORTH MAIN ST. SALEM, UT 84653 | CALL US TOLL-FREE 855-770-4002