Within the last few months, a number of medical studies have been published stating that patients who have tested positive for COVID-19 are experiencing long lasting neurological problems. These range from headaches, brain fog, memory loss, vertigo, and confusion to stoke and/or coma. One study from Wuhan China showed 45% of patients with severe COVID-19 sickness experienced marked neurological issues1. A study from France showed 84% of ICU patients experienced residual poor attentions and difficulty with decision-making and controlling behavior2. One recent study from Shanghai China showed that even mild cases of COVID-19 caused micro-structural changes in the brain matter based on MRI images taken 3 months post recovery3. These neurological conditions are as a result of traumatic brain injury (TBI). As with other viral infections, inflammation of the brain can occur as well as an inflammatory condition known as Acute Disseminated Encephalomyelitis (ADEM) which affects the brain and spinal cord. With TBI symptoms becoming something that COVID-19 patients have to look forward to post recovery, is there any current treatments that could possibly help those recover from these long lasting neurological problems?
Currently there are very few treatment options available to treat traumatic brain injuries whether they occur from a viral infection (COVID-19) or physical trauma (Concussions).
Some treatments, such as attention training, cognitive behavioral therapy, working memory, and mindfulness meditation have demonstrated moderate efficacy in managing specific cognitive symptoms. Other trials have failed to demonstrate efficacy, especially in more severe brain injuries.
Pharmacological treatments, including progesterone have failed to effect neurological and functional outcome where most did not improve clinical outcomes when advanced to late-stage clinical trials.
Non-pharmacological treatments, such as hyperbaric oxygen therapy (HBOT), has had mixed results. HBOT has shown to be successful when administered in the acute phase (first 48 hours)4, whereas if administered later on there was no evidence that supported the application of hyperbaric oxygen showed no improvement in quality of life after TBI5. Recent case reports show that HBOT may improve hypoxemia in severe COVID-19 patients6. We hypothesize that this could possibly assist in the treatment of TBI in patients if administered early on. Unfortunately, HBOT is not widely available and is still considered experimental treatment for both COVID-19 and TBI.
There are two therapeutic modalities within the TruDenta Rehabilitation program that have been shown to restore cognitive function and help eliminate the symptoms associated with TBI with little to no negative side effects. These two modalities, which have shown promising results on TBI patients and could potentially reduce post SARS-CoV2 symptoms, are Photobiomodulation (PBM) and Cranial Electrotherapy Stimulation (CES).
Photobiomodulation therapy (PBM) is defined as a form of light therapy that utilizes non-ionizing light sources (LEDs, lasers, and/or broadband light). These lights are generally red (630-660nm), infra-red (730-980nm), with blue (405-470nm) added in occasionally. The lights stimulate cells to generate more energy (ATP) and undergo self-repair. You may have seen photobiomodulation devices used in the neonatal center of your local hospital for the treatment of jaundice. They can also be found in the facial care isle of your local market is devices for treating acne and fine wrinkle removal. PBM is generally used for wound disinfection, tissue repair, inflammation reduction, pain relief, and accelerated wound healing. Treatments are generally short (2-10 minutes) and can vary in the amount of treatments needed in order to achieve optimum results. PBM is a non-invasive treatment and is FDA cleared.
PBM is becoming increasingly widespread throughout the world and is considered a standard of care for some cancer related issues7. PBM has been shown to be effective for TBI delivered during the acute phase up to 8 years after the injury occurred. These studies have shown that PBM may stimulate both neurogenesis (the ability of the brain to repair itself) and synaptogenesis (encourage cells to form new synaptic connections). Improvements in cognitive function include improved concentration, memory recall, better sleep, fewer post-traumatic stress disorder symptoms and a better ability to control social behavior 8,9,10,11.
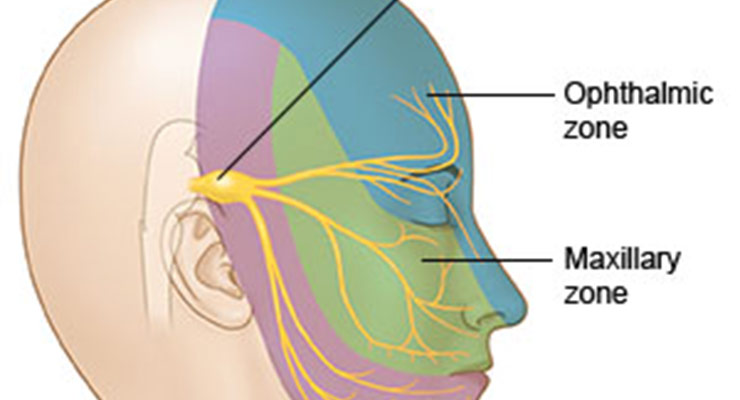
Cranial Electrotherapy Stimulation (CES) is the term used for medical treatment where small amounts of electricity, at the level of microcurrents, is passed thorough the brain to normalize and bring back balance back to the brain’s electrochemistry, which can be thrown into disarray by trauma whether it be physical, psychological or viral. CES is used for the treatment of PTSD, anxiety, insomnia, depression, headaches and addiction recovery. It is currently used by the US military in VA hospitals across the nation by the US Navy in their pain management program. CES is generally administered by placing small electrodes on the lobes of the ears to deliver the electrical pulse to the brain. By placing the electrodes on the ears allows the electrical pulses to be administered at a very low level (microcurrent).
CES has been shown to provide a non-drug way of inducing sleep and relaxation with a substantial reduction of anxiety. In TBI patients that have experienced seizures, CES has shown to reduce the number of episodes while being treated12. While seizures have not been widely reported in the past 5 months since the onset of COVID-19 pandemic, it is plausible to expect seizures to happen in these patients13.
In one particular TBI case, the combined treatment of Photobiomodulation and Cranial Electrotherapy Stimulation allowed the 13 year old patient who had suffered from moderate TBI go from having extreme light and sound sensitivity, mood swings and the inability to stand without vertigo to being able to be cleared to return to school 7 days after the combined treatment began. 10 months later the teen had no had any relapses nor does he experience any headaches or mood swings attributed to TBI.
Unfortunately, our understanding of the neurological consequences of COVID-19 remains in its early stages. A number of studies are currently being performed with PBM devices on severe COVID-19 patients and CES treatment on post COVID-19 patients. We cannot say for sure that the modalities can restore normal fuction back to a post-covid patient, but we are confident that since these two modalities show their effectiveness in reducing inflammation and restoring normal electrical, cellular and cognitive function to patients suffering from physical TBI that COVID-19 TBI symptoms should not be much different in treatment.
If you or anyone you know is experiencing TBI symptoms after your fight with COVID-19 give one of our 400+ doctors in the US and Canada a call and schedule a consultation with them today. Let us help you restore normal function and help you get your life back.
-
- Neurologic Manifestation of Hospitalized Patients with Coronavirus Disease 2019 in Wuhan, China:
JAMA Neurol. 2020;77(6):683-690. doi:10.1001/jamaneurol.2020.1127
https://jamanetwork.com/journals/jamaneurology/fullarticle/2764549
- Neurologic Features in Severe SaRA-CoV2 Infection:
June 4, 2020 N Engl J Med 2020; 382:2268-2270 DOI: 10.1056/NEJMc2008597
https://www.nejm.org/doi/full/10.1056/NEJMc2008597 - Cerebral Micro-Structural Changes in COVID-19 Patients – An MRI-based 3-month Follow-up Study:
August 03, 2020 DOI:https://doi.org/10.1016/j.eclinm.2020.100484
https://www.thelancet.com/journals/eclinm/article/PIIS2589-5370(20)30228-5/fulltext#.Xyig6jaBrFk.twitter - Hyperbaric oxygen therapy for reduction of secondary brain damage in head injury: an animal model of brain contusion:
J Neurotrauma. 2004;21:41–48. PMID: 14987464 DOI: 10.1089/089771504772695931
https://pubmed.ncbi.nlm.nih.gov/14987464/ - Hyperbaric oxygen therapy for the adjunctive treatment of traumatic brain injury.
Cochrane Database Syst Rev. PMID: 23235612 DOI: 10.1002/14651858.CD004609.pub3
https://pubmed.ncbi.nlm.nih.gov/23235612/ - Hyperbaric oxygen therapy may be effective to improve hypoxemia in patients with severe COVID-2019 pneumonia: two case reports
Undersea Hyperb Med . Second-Quarter 2020;47(2):181-187.
https://pubmed.ncbi.nlm.nih.gov/32574433/ - Photobiomodulation Therapy in the Treatment of Oral Mucositis, Dysgeusia and Oral Dryness as Side-Effects of Head and Neck Radiotherapy in a Cancer Patient: A Case Report
Dent J (Basel). 2018 Dec; 6(4): 64.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6313426/ - Transcranial Low-Level Laser (Light) Therapy for Brain Injury
Photomed Laser Surg. 2016 Dec 1; 34(12): 587-598
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5180077/ - Shining Light on the Head: Photobiomodulation for Brain Disorders
BBA Clinical Volume 6, December 2016, Pages 113-124
https://www.sciencedirect.com/science/article/pii/S2214647416300381 - Photobiomodulation for Traumatic Brain Injury and Stroke
J Neurosci Res. 2018 Apr, 96(4); 731-743
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5803455/ - Transcranial Photobiomodulation Therapy in the Cognitive Rehabilitation of Patients with Cranioencephalic Trauma
Photobiomodul Photomed Laser Surg, 2019 Oct 1; 37(10); 657-666
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6818475/ - CES For Mild Traumatic Brain Injury
Practical PAIN MANAGEMENT, July/August 2008; 70-77
https://www.stress.org/wp-content/uploads/CES_Research/kirsch_brain_injury.pdf - The use of cranial electrotherapy stimulation in the treatment of closed-head-injured patients
Journal of Brain Injury – Pages 357-361 | Received 12 Oct 1992, Accepted 10 Apr 1993, Published online: 03 Jul 2009
https://www.tandfonline.com/doi/abs/10.3109/02699059409150986 - Seizures associated with coronavirus infections
Seizure, 2020 Jul; 79; 49-52
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7212943/
- Neurologic Manifestation of Hospitalized Patients with Coronavirus Disease 2019 in Wuhan, China: