
Compendium Magazine
Published by AEGIS Communications
By Charles W. Martin, DDS
Abstract
An innovative assessment and treatment protocol system now enables dentists to more effectively and comprehensively assess and treat patients with chronic headache and migraine pain, as well as other dental force–related conditions. The system combines objective assessment with scientifically based, systematic, and predictable treatment methods and technologies to offer successful outcomes and maintenance.
Among the most prevalent reasons that patients visit the dental office are treatment for toothaches, broken or chipped teeth, and bleeding gums. Patients also frequently visit dentists seeking relief from headaches, many of which could be the result of dentomandibular sensorimotor dysfunction, a disorder of the head and neck, temporomandibular joints (TMJ), jaw function, and dental forces. This dysfunction is the underlying cause of both symptomatic and asymptomatic conditions, which may include, but are not limited to, tooth wear, bruxism, repeatedly fracturing restorations, TMJ disorders, chronic headaches and migraines, and numerous other problems.1-3
Chronic headaches, migraines, and TMJ disorders afflict millions of people, and their effects can be quite devastating and debilitating. Approximately 90% of the population experiences headaches, and individuals who suffer from migraines lose between 157 million days of school and work annually.4 Additionally, the National Institute of Dental and Craniofacial Research (NIDCR) has estimated that the number of Americans who suffer from TMJ disorders surpasses 10 million. The projection of how many individuals actually have some form of a TMJ problem could be closer to 15 to 45 million.5
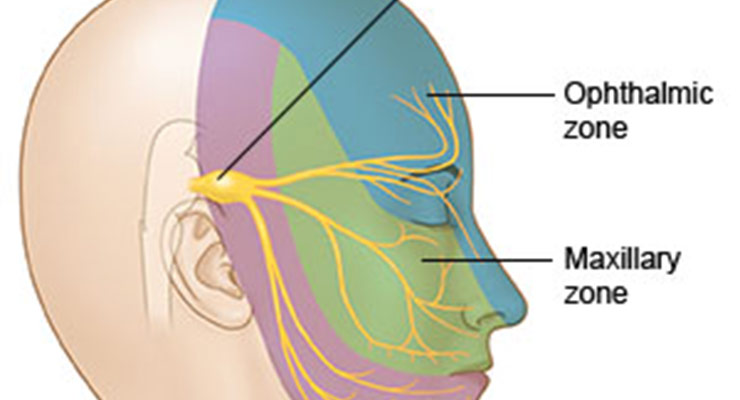
Headache pain is mediated by the trigemino-cervical nucleus and results from aggravating stimulation of the nerve endings that unite the head, neck, mouth, and shoulder area, or from irritation of the nerves themselves.6 Referred pain from disorders in the dentomandibular regions also can be perceived as headache.7
The effect of unbalanced or overloaded muscle forces related to sensorimotor and somatosensory proprioceptive or nociceptive physiology is intimately linked to the trigeminal nerve.1,3,8 The role of the trigeminal nerve, the largest and most complex of the cranial nerves, is well recognized among orofacial pain and temporomandibular joint disorders.9 The mandibular or third division of the trigeminal nerve sends afferent and efferent fibers to the masticatory muscles, and also refers pain to other areas within its branches, such as the maxilla.10
The pathway of circuits, reflexes, motor control, proprioceptive and nociceptive processes, and referred pain perpetuate dentomandibular sensorimotor dysfunction.3 Individuals with dentomandibular sensorimotor dysfunction likely have multiple trigger points surrounding the head, neck, and jaw, and the nociceptive input from peripheral tender muscles can cause central sensitization and chronic headache conditions.11
The areas similarly controlled by the brachial arch cranial nerves, which begin in the brain stem, constantly receive nerve signals. Injuries, trauma, or inflammation to the dentomandibular and craniofacial tissues therefore affect transmission, modulation, and adaptation of nociceptive signals in the brain stem, which underlies pain in the face, mouth, and head.12
Dentists who are appropriately trained and expert in the diagnosis and treatment of chronic headaches, migraines, and TMJ disorders13,14 are increasingly taking a more active and prevalent role in assessing and treating dental force–related problems. They are doing so by combining new programs, systems, and technologies adapted from other healthcare disciplines. For instance, for several years, low-level laser therapy, therapeutic ultrasound, and microcurrent nerve stimulation have been used in sports medicine as methods of treatment to enhance, hasten, and improve the recovery of athletes suffering from musculoskeletal and force-related injuries.15
Structures innervated by certain trigeminal branches are known to cause headache—including the muscles, joints, and ligaments in the mandible and maxilla. The role of dentomandibular sensorimotor dysfunction in headache pain becomes obvious.16 Establishing normal function and relieving patients of pain symptoms requires that the neurology, muscle activity, and brain chemistry be reset.12,17
Innovative Diagnostic and Treatment Technology
Along with systematic and objective assessment and monitoring, as well as neuroscience, innovative sports medicine approaches and technologies now are increasingly becoming a part of dentistry. They are being employed to successfully address headaches associated with dental force–related complaints.14-20
Currently, dentists can assess and, along with their dental teams, treat and manage the headache and dental force–related conditions of their patients through a comprehensive system (TruDenta®, Dental Resource Systems, Inc., www.trudenta.com). This proprietary, patented system (Figure 1), which incorporates assessment and treatment hardware and software, is designed to provide predictable, reliable, and durable relief from pain, improved functional and/or restorative dental results, and overall well-being and improved quality of life for patients experiencing chronic and migraine headaches and other symptoms of dentomandibular sensorimotor dysfunction.
The system enables dentists to deliver a visually engaging assessment, and their dental teams can participate in extending scientifically proven treatments for patients who are suffering from dentomandibular sensorimotor dysfunction. These technological equipment and treatment methods have been approved by the Food and Drug Administration (FDA), and the system’s assessment protocol adheres to American Medical Association (AMA) guidelines. The examination and evaluation component of the system is composed of a head health, medical, headache history, and pharmacological assessment. Afterwards, these findings are combined with a standard-of-care panoramic radiographic examination. In addition, dental, occlusal, orthodontic, periodontal, and airway examinations also are recommended and encouraged.
The examination and the assessment devices objectively measure and visually display the reason(s) for the symptoms. Using this patented system allows dentists and their dental teams to comprehensively approach the therapy that would be required for dental foundation or bite imbalance. The functional elements of the head, neck, and oral cavity are addressed thoroughly.
With digital range of motion (ROM) testing, for instance, a dental team is able to capture and measure the cervical range of motions, as expressed in the patient’s head movement. This computerized measurement allows dentists to study the head movement, which is connected to jaw movement. This connection has an effect on the proprioceptive feedback system of the dental occlusion, the temporomandibular joints, and the muscles of mastication.
Another important tool in the system is the T-Scan, which can be used prior to and during the rehabilitation. The T-Scan is relied upon to evaluate imbalances in the teeth, joints, and muscles, or the dental foundation. Apart from complementing and supporting the assessment opinion, these objective data instruments are helpful in earning a patient’s acceptance of the treatment plan.
During the comprehensive examination, the dentist is able to locate and identify early warning signs in the mouth that might predict and forecast dysfunction conditions and disease in other anatomical parts. Among the dysfunction conditions are maladies such as headaches and migraines, tinnitus, sleep disorders, compromised airway control, and range-of-motion (ROM) and postural adaptations that have been restricted. At the root of these conditions and symptoms is dentomandibular sensorimotor dysfunction, which results from unmanaged and unbalanced muscle forces.1,3,8
Dentists perform the assessment stages of the patients’ examinations, and dental staff members perform the rehabilitative treatments. Continuing education training in the proprietary system is available to dentists and their dental teams at the University of Nevada Las Vegas or NOVA Southeastern University dental schools. According to company data, when adhered to correctly, this unique approach to addressing dentomandibular sensorimotor dysfunction has been 93% effective in relieving symptoms of pain for properly diagnosed cases.
Case Presentation
A 52-year-old woman presented complaining of various symptoms of dentomandibular sensorimotor dysfunction. As with any assessment and clinical treatment protocol, the first step was determining the condition(s) that could be amenable to treatment. The patient also received a complete examination, which included a head health, medical, and headache history, as well as a pharmacological assessment. Dental, periodontal, airway, orthodontic, and occlusal examinations also were undertaken.
The patient showed symptoms of bilateral frontal headaches described as pressure and achy type headaches. Among her comments: she said she had pain all day long most days; felt her left ear was “plugged up”; and that her “smile muscles” hurt a lot. She indicated that she experienced occipital and temporal head pain; her mandibular range of opening was within normal range. She had sought help from a chiropractor 3 years earlier as well as an allergist, who had given her allergy medications.
The patient reported no allergies to any medications. She did report occasionally taking over-the-counter pain medications, including aspirin and Aleve™ (Bayer, www.aleve.com), for her arthritis. She said she took the beta-blocker nadolol, 50 mg, for hypertension. The patient was also taking the angiotensin-converting enzyme inhibitor lisonpril 12.5 mg for her hypertension and the selective serotonin re-uptake inhibitor (SSRI) citalopram (Celexa®, Forest Laboratories, Inc, www.frx.com), 20 mg once a day, as prescribed for depression.
In addition to frequently experiencing jaw pain when chewing, talking, and at rest, she noted jaw clicking, teeth clenching, and grinding, as well as limited ROM of the neck, along with shoulder pain and stiffness.
Upon palpitation, the patient showed tenderness of the anterior temporalis bilaterally, and the superficial masseter, trapezius neck/shoulder area, the sub-occipital, masseter, pterygoid, and sternocleidomastoid (SCM) were moderately to severely sensitive. The patient rated the pain a 7 out of a pain scale of 1 to 10, with 10 being the worst. Severe tenderness also was detected upon palpation of the lateral capsules of the TMJ bilaterally. In brief, all of the muscles of mastication and TMJ ligaments produced definitive myalgia, which negatively altered her normal daily living and social habits.
Crucial to establishing the severity of sensorimotor dysfunction, any abnormal, excessive, or imbalanced forces were identified objectively using mandibular ROM disability, cervical ROM disability (digitally), and digital force analysis (TruDentaScan). These technologies were combined with cone beam computed tomography (CBCT) radiographs. It is important to note that the ROM portion of the diagnostic process provides objective data conforming to American Medical Association (AMA) guidelines.
The patient’s T-Scan testing showed that 44.6% of the pressure from her bite was localized to the left side of her mouth; the right side of her mouth received 55.4% of biting pressure (Figure 2 and Figure 3). This demonstrated a slight imbalance of the stomatognathic system, which adversely impacted her overall well being.
Clinical examination revealed right TMJ crepitus upon opening and closing. Cervical ROM measurements showed pain on extension and limited extension (Table 1). The patient presented with forward head posture, a back sleeping position, and a sitting and standing work position. A digital ROM study revealed extension of the neck limited to 43 degrees (60 degrees is the normal ROM). Flexion test revealed movement of 38 degrees (normal is 50 degrees). The patient’s left lateral was at 34 degrees, and right lateral movement was 37 degrees (45 degrees is the normal neck stretch). Her rotational movements were left 58 degrees and right 70 degrees (80 is the normal rotational movement). These findings were considered likely to account for the moderate to severe pain at the occipital, trapezius, and SCM muscles.
Assessment
Based on assessment codes that are in agreement with the AMA insurance codes, it was determined that the patient suffered from the following: atypical face pain, cervicalgia, eye pain/pressure, headache, laxity of the TMJ ligament, TMJ pain, muscle spasms, and myalgia.
Treatment Protocol
Treatment was directed toward conservative therapy in an attempt to avoid surgery, establish orthopedic realignment of the mandible, improve myalgia and forward head posture, reduce inflammation, strengthen the musculoskeletal system, and alleviate headaches, as well as pain, pressure, and sensitivity in the eyes. Further treatment recommendations, all of which conform to the AMA insurance codes, consisted of office visits, manual muscle testing, ROM testing, TMJ ultrasound, applied electrical stimulation, manual muscle therapy, cold laser therapy, therapeutic exercises, home care instructions, occlusal analysis, occlusal orthopedic device (NU modifier), and self-care home management training.
Stabilization goals included maintaining muscle comfort, joint stability, and orthopedic stabilization of the mandible. This normal function was achieved through an occlusal orthopedic device. Unlike a bruxing guard, the occlusal orthopedic device is a medical-grade orthotic for the mouth that helps to balance, stabilize, and support the mandible.
It was important to ensure that the orthotic was fabricated in a manner that improved the jaw position to minimize the patient’s pain and symptoms. This was accomplished through electrical stimulation, manual muscle therapy, and cold laser therapy. These methods helped promote blood flow to the tense muscles of mastication. This blood flow, in return, relaxed the muscles so that when impressions, bite registrations, and casts of the mouth were fabricated, they were created in the proper relaxed (versus tense) position. Consequently, it was then possible to make the orthotic to position the mandible in this relaxed and healthy position.
The patient was taught therapeutic exercises by the dental staff. These exercises first were done in-office, and then continued by the patient at home. The importance of continuing the regimen at home was emphasized to the patient. If treatment did not continue after the patient left the office, she would not progress in her care.
Treatment Outcome
The patient’s treatment consisted of 12 weekly in-office visits of therapeutic rehabilitation using cold laser therapy, ultrasound therapy, low-level electrical current stimulation, and manual muscle therapy. In addition to fabricating a custom rehabilitation orthotic for the mouth, three sequential occlusal equilibrations—ie, bite adjustments—were performed to correct bite imbalances.
At 12 weeks, the patient’s health and stability were confirmed with a digital ROM test. ROM values were found equal to or above physiologic norms (Table 1). Dental bite force balance also was confirmed with the T-Scan analysis (Figure 4 and Figure 5); it revealed left/right balance at 49.8%/50.2%, which was well within physiologic norms and tooth force readings at normal levels. Her headaches and constant daily pain were gone, except for an occasional flare-up managed with her exercises.
Conclusion
Acceptance and utilization of an innovative assessment and treatment protocol system that employs objective and subjective methods and technologies has expanded dental practice capabilities. By adapting knowledge and techniques from fields such as sports medicine, dentists and their dental staffs can more effectively and comprehensively assess and treat patients with chronic headache and migraine pain, as well as other dental force–related conditions.
Dentists are able to assess and review the functional elements of the head, neck, and oral cavity in a manner that can identify and correct the actions of the musculoskeletal and dentomandibular health. All therapy for bite imbalance, as well as dental foundation, can be approached in a comprehensive and complete manner that addresses all underlying foundational elements. The proprietary system provides dentists and their dental teams with a visually powerful and objective assessment. When coupled with scientifically based, systematic, and predictable treatment methods and technologies, the long-term treatment and rehabilitation outcome is successful.
About the Author
Charles W. Martin, DDS Private Practice, Richmond, Virginia
References
- Junge D. Oral Sensorimotor Function. New Haven, MO: Medico Dental Media International, Inc; 1998.
- Okeson JP. Management of Temporomandibular Disorders and Occlusion. 6th ed. St. Louis, MO: Elsevier Mosby; 2008.
- Sessle BJ. Mechanisms of oral somatosensory and motor functions and their clinical correlates. J Oral Rehabil. 2006;33(4):243-261.
- Headache. US News and World Report Web site. Accessed November 20, 2013.
https://health.usnews.com/conditions/pain-management/headache - Adult Data & Statistics. National Institute of Dental and Craniofacial Research Web site. Accessed November 20, 2013.
https://www.nidcr.nih.gov/research/data-statistics/adults - Bogduk N. Anatomy and physiology of headache. Biomed Pharmacother. 1995;49(10):435-445.
- Bogduk N. The neck and headaches. Neurol Clin. 2004;22(1):151-171, vii.
- Montgomery MW, Shuman L, Morgan A. T-scan dental force analysis for routine dental examination. Dent Today. 2011;30(7):112-114, 116.
- Shankland WE 2nd. The trigeminal nerve. Part I: An over-view. Cranio. 2000;18(4):238-248.
- Shankland WE 2nd. The trigeminal nerve. Part IV: the mandibular division. Cranio. 2001;19(3):153-161.
- Fernández-de-las-Peñas C, Cuadrado ML, Arendt-Nielsen L, et al. Myofascial trigger points and sensitization: an updated pain model for tension-type headache. Cephalalgia. 2007;27(5):383-393.
- Sessle BJ. Recent insights into brainstem mechanisms underlying craniofacial pain. J Dent Educ. 2002;66(1):108-112.
- Headache Topic Sheet. National Headache Foundation Web site. Accessed November 20, 2013.
https://headaches.org/2012/10/25/migraine/ - Dentists: Doctors of Oral Health. American Dental Association Web site. Accessed November 20, 2013.
https://www.ada.org/en/about-the-ada/dentists-doctors-of-oral-health - Cameron MH. Physical Agents in Rehabilitation. 3rd ed. St. Louis, MO: Elsevier Saunders; 2009.
- Bogduk N. The anatomical basis for cervicogenic headache. J Manipulative Physiol Ther. 1992;15(1):67-70.
- Sessle BJ. Peripheral and central mechanisms of orofacial inflammatory pain. Int Rev Neurobiol. 2011;97:179-206.
- Öz S, Gökçen-Röhlig B, Saruhanoglu A, Tuncer EB. Management of myofascial pain: low-level laser therapy versus occlusal splints. J Craniofac Surg. 2010;21(6):1722-1728.
- Marini I, Gatto MR, Bonetti GA. Effects of superpulsed low-level laser therapy on temporomandibular joint pain. Clin J Pain. 2010;26(7):611-616.
- Srbely JZ, Dickey JP. Randomized controlled study of the antinociceptive effect of ultrasound on trigger point sensitivity: novel applications in myofascial therapy? Clin Rehabil. 2007;21(5):411-417.
Additional Resources
As noted, patients frequently visit dentists seeking relief from headaches, many of which could be the result of dentomandibular sensorimotor dysfunction, a disorder of the head and neck, temporomandibular joints (TMJ), jaw function, and dental forces. Chronic headaches, migraines, and TMJ disorders afflict millions of people, and their effects can be quite devastating and debilitating. Other related content on this subject can be found at Compendium’s website. Examples include the following:
Managing Craniofacial Pain the Multi-Disciplinary Way
https://www.aegisdentalnetwork.com/cced/2012/03/managing-craniofacial-pain-the-multidisciplinary-way?q=
Patterns of Use for an Enhanced Nociceptive Trigeminal Inhibitory Splint
https://www.aegisdentalnetwork.com/id/2011/12/patterns-of-use-for-an-enhanced-nociceptive-trigeminal-inhibitory-splint?q=
What’s Hiding Behind the Smile?
https://www.aegisdentalnetwork.com/id/2012/10/whats-hiding-behind-the-smile?q=
Using Computer-Guided Surgery for Partial Guidance of Zygoma Implants
https://www.aegisdentalnetwork.com/cced/2012/10/using-computer-guided-surgery-for-partial-guidance-of-zygoma-implants?q=





 © 2025 - NATIONAL DENTAL SYSTEMS, INC. | 430 NORTH MAIN ST. SALEM, UT 84653 | CALL US TOLL-FREE 855-770-4002
© 2025 - NATIONAL DENTAL SYSTEMS, INC. | 430 NORTH MAIN ST. SALEM, UT 84653 | CALL US TOLL-FREE 855-770-4002