
Dentistry Today Magazine
By Robert L. Harrell, DDS
Dentomandibular sensorimotor dysfunction(DMSD)
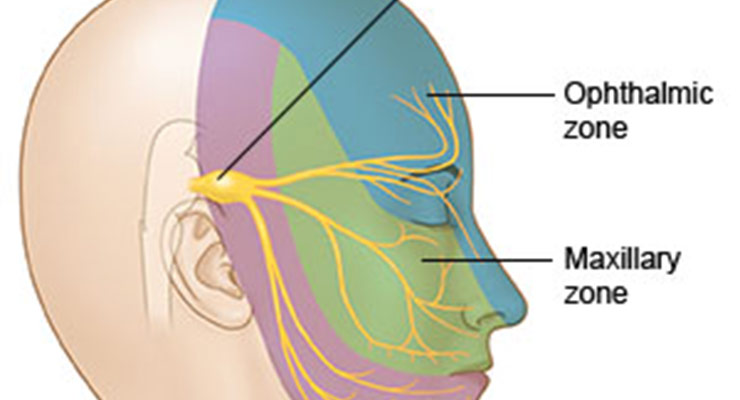
Dentomandibular sensorimotor dysfunction(DMSD) is associated with such conditions as chronic headaches, migraines, temporomandibular joint (TMJ) disorders, and numerous other symptoms. When no definitive pathology exists, more emphasis has been devoted to the masticatory muscles, soft tissues in the head and neck area, and altered central nervous system pain processing in the trigeminal area. Dentists are trained and expert in assessing and treating the anatomical areas affected by these conditions and can provide patients with dental headache care, pain resolution, and treatment of force related problems.
This article reviews the need for providing care to patients with chronic and unresolved headache pain. It also demonstrates the typical use of a complete, proprietary system (TruDenta [Dental Resource Systems]) for providing comprehensive assessment, treatment, and management protocol to achieve consistent, long-lasting, and effective relief from pain and dental foundation rehabilitation.
For millions of Americans affected by DMSD, pain is part of their daily lives. Dentomandibular sensorimotor dysfunction— a disorder of the head and neck, TMJs, jaw function, dental forces, and neurology of these structures and functions resulting from imbalanced or improper forces—lies at the root of many conditions. These include, but are not limited to: chronic headaches, migraines, TMJ disorders, and numerous other symptoms, such as TMJ sounds or vibrations (eg, clicking and popping of the jaw), and pain in the head, neck, face, or jaw.1,2
The scope and negative impact of these conditions are significant. According to the National Headache Foundation, an estimated 90% of the population suffers from headaches, with migrane sufferers losing more than 157 million work and school days a year because of heachace pain.3More than 29 million Americans suffer from migraines.4 Additionally, the National Institute of Dental and Craniofacial Research indicates that anywhere from 10 to 45 million Americans suffer from some type of TMJ issue.5
Finding little or no relief from over-thecounter medications or nonpharmacological techniques, thousands of patients look to different healthcare professionals for treatment solutions to their often debilitating pain. Dentists, trained and knowledgeable in assessing and treating the anatomical areas affected by these conditions, are uniquely suited to offer such patients dental headache care, pain resolution, and treatment of force related problems.6-8
Assessment Tools And Treatments From Other Disciplines
Dentistry has applied many technological and material science innovations to assess and treat oral-based problems. Highstrength ceramics or in-office CAD/CAM systems address the need to restoratively correct the destructive effects of wear, bruxism, and tooth decay.9,10 The development of such enhanced materials has been based on clinical and research knowledge of the effects of the oral environment on restoration longevity, natural teeth opposition, and the masticatory system.11
Cervical range of motion (CROM) devices or occlusal analysis equipment (TScan) have helped shed light on possible functional and physiological issues influencing the dentomandibular area and/or contributing to related health problems.12-16 Dentists have applied these technologies to implant procedures and restorative rehabilitations centering on occlusal adjustments. For instance, electronic axiographic tracers are used to resolve the movements of the condyles; magnetic resonance tomography imaging can be utilized to analyze the anatomical relation of joint surfaces to the disc;14 and pressure sensitive foils in conjunction with time resolution enable an accurate analysis of masticatory forces.11-13
These assessment and restorative approaches have contributed to greater comprehension of the interrelationship be tween force overload and disease/dysfunction within the oral environment and the masticatory system. In restorative dentistry, awareness of the symptoms of malocclusion has been key to offering predic table, consistent, and durable dental treatments.11,17
When malocclusion (ie, abnormal forces between some or all of the dentition resulting in pain and/or damage to the tooth anatomy or periodontal interface) is present, alterations and adaptations may occur to the masticatory musculature, the TMJ, and the function of the condyle.18-22 These adaptations sometimes may contribute to acute or chronic pain in the head and neck region served by the trigeminal cervical nucleus. Subsequently, this can lead to additional neurochemical adaptations and compensatory muscle activity that can limit range of motion (eg, cervical or mandibular) and/or result in trigger point muscle spasms.20,21,23-25
When the occlusion is force balanced, a person is comfortable at rest and in full closure, exhibits mandibular range of motion within normal limits, and is free from acute or chronic pain. The person demonstrates normal tooth anatomy and mobility, normal posture and work abilities, and has no dietary restrictions due to dental function limitations.11,26-29
Practical measuring instruments have successfully identified occlusal interferences and heavier forces, as well as muscle responses and pain symptoms during masticatory function. 26-28 Technology has helped to accurately show significant discrepancies in jaw position and muscle function that contribute to chronic daily headaches.30 Such objective data concerning pain stimuli, in conjunction with masticatory function combined with research on TMJ, orofacial, headache, and other systemic pain responses related to muscle forces, have shifted how dentistry deals with patients experiencing debilitating discomfort issues.
When there is no definitive tissue pathology, more emphasis has been devoted to understanding that pain in some patients may arise from altered central nervous system pain processing, especially in the masticatory muscles and soft tissues in the head and neck area.31 Heightened muscle tension and force—as related to parafunctional habits and stress—signal the likelihood of jaw and facial pain.32 Many types of headaches are now understood to be referred pain from myofacial trigger points in the posterior cervical, head, and shoulder muscles.33
Reversing parafunctional habits (eg, bruxing, clenching, and grinding) through behavior modification has proven effective in minimizing pain from TMJ disorders and myofacial issues.34,35 Deprogrammers have played a role in “retraining” the masticatory muscles, recognizing the muscles’ role in the forces contributing to pain, as well as the fact that controlling the perpetuating factors (ie, force) can help control, reduce, or eliminate pain.35,36
For years, sports medicine technologies (eg, low-level laser therapy, therapeutic ultrasound, and microcurrent nerve stimulation) have been used successfully to enhance, accelerate, and improve athletes’ recovery from musculoskeletal and force related injuries.37 Such treatment methods—when combined with neuroscience and systematic and objective assessment/monitoring—now are being increasingly applied in dental practices.38-42
A Comprehensive And Innovative System
The availability of a patented, proprietary system (TruDenta) enables dentists to provide comprehensive assessment, treatment, and management protocol to achieve consistent, long-lasting, and effective relief from pain and dental foundation rehabilitation for patients suffering from the symptoms of DMSD. The system incorporates proven combinations of sports medicine rehabilitation and advanced dentistry techniques, as well as well-developed and tested equipment, technology, software, and therapeutic protocols (Figure 1). These have been cleared by the FDA. They also have been shown to objectively measure and visually illustrate the cause of patient symptoms relating to DMSDs, as well as contribute to predictable outcomes when combined with conservative care.38-42- 45
The system uses T-Scan technology (TruDentaScan digital force measurement) for evaluating the amount and balance of forces at closure and while chewing, and a computerized ROM assessment tool (TruDenta – ROM), which measures the CROM as expressed in the patient’s head movements. A CROM disability can be correlated with mandibular ROM disability and/or an imbalance in the dental foundation. The system’s rehabilitation technology features therapeutic ultrasound, transcutaneous electrical stimulation (ie, subthreshold microcurrent), low-level laser therapy, and intraoral orthotics.
The following case demonstrates the typical TruDenta assessment and treatment protocol for individuals presenting with chronic headache pain and other discomfort resulting from DMSD.
Case Report
Diagnosis and Treatment Planning A 36-year-old woman presented, complaining of various symptoms of DMSD. As with any assessment and clinical treatment protocol, the first step was determining the condition(s) that may be amenable to treatment. Therefore, the patient completed—and the dentist reviewed—comprehensive head health, medical, and headache history. A review of the patient’s pharmacological treatments also was undertaken prior to the clinical evaluation. Dental, periodontal, airway, orthodontic, and occlusal examinations also were undertaken. Additionally, a computed tomography scan had been done recently by her neurologist to rule out the existence of any underlying organic condition.
The patient showed symptoms of bilateral frontal headaches. She experienced occipital and temporal head pain, jaw pain bilaterally with opening and closing, and limited mandibular ROM with limited vertical opening. In addition to frequently experiencing jaw pain when chewing, talking, and at rest, she noted jaw clicking, teeth clenching, and grinding, as well as recurring eye pain, pressure behind the eyes, and shoulder pain and stiffness.
The patient was allergic to codeine and reported taking over-thecounter pain medications (eg, Tylenol [McNeil Consumer Healthcare]; Advil [Wyeth]; and Aleve [Bayer]), which did not provide relief. She also reported taking a prescription antihistamine medication (Allegra [Perrigo Company]) for seasonal allergies. Additionally, she reported seeking the care of an oral surgeon after awakening one morning with a locked jaw. The oral surgeon had recommended joint surgery.
Upon muscle palpation examination, the patient showed tenderness of the anterior and middle bands of the temporalis muscle. In addition, bilaterally, the masseter, occipital, and trapezius neck/shoulder area, pterygoids, and sternocleidomastoid were severely sensitive. The patient rated the pain a 10 on a pain scale of one to 10, with 10 being the worst. Severe tenderness also was detected upon palpation of the posterior and lateral capsules of the TMJ. In brief, all of the muscles of mastication, TMJ ligaments, and of the jaw position produced stark myalgia, which negatively altered her normal daily living and social habits.
Crucial to establishing the severity of sensorimotor dysfunction, any abnormal, excessive, or imbalanced forces were identified objectively using mandibular ROM disability, cervical range of motion disability (digitally), and digital force analysis (TruDentaScan). These technologies were combined with panoramic radiographs. It is important to note that the ROM portion of the diagnostic process provides objective data conforming to AMA guidelines.
The patient’s T-Scan testing showed that 38.5% of the pressure from her bite was localized to the left side of her mouth; the right side of her mouth received 61.5% of biting pressure (Figure 2). This demonstrated an imbalance of the stomatognathic system, which adversely impacted the patient’s overall well being.
Clinical examination revealed bilateral crepitus upon opening and closing. Cervical ROM measurements showed pain on extension and limited extension. The patient presented with forward head posture, a back sleeping position, and a sitting and standing work position. A digital ROM study revealed extension of the neck limited to 50° (60° is the normal ROM). The patient’s left lateral rotation was at 37° (45° is the normal neck stretch) (Figure 3). These findings were thought to likely account for the severe pain at the occipital, trapezius, and SCM muscles.
Based on assessment codes that are in agreement with the AMA insurance codes, it was determined that the patient suffered from the following: atypical face pain, cervicalgia, eye pain/pressure, headache, limited mandibular ROM, TMJ pain, muscle spasms, and myalgia.
Treatment Protocol
Treatment was directed toward conservative therapy in an attempt to avoid surgery, establish orthopedic realignment of the mandible, im – prove myalgia, reduce inflammation, strengthen the musculoskeletal system, and alleviate headaches as well as pain, pressure, and sensitivity in the eyes. First steps in the treatment process would involve assessment conforming to AMA insurance codes, would include manual muscle testing, TMJ ultrasound, and ROM testing. Then, an individualized treatment plan would involve therapeutic in-office appointments consisting of applied electrical stimulation, manual muscle therapy, cold laser therapy, and therapeutic ultrasound. Additional components of the weeks-long therapy to be incorporated would be therapeutic exercises, an occlusal orthopedic device, and self-care home management training, based on periodic occlusal analysis.
Stabilization goals were directed toward maintaining muscle comfort, joint stability, and orthopedic stabilization of the mandible. This normal function restoration was achieved through an occlusal orthopedic device or rehabilitation orthotic. The rehabilitation orthotic helps to balance, stabilize, and support the mandible. At the time she presented, the patient experienced symptoms from an injured TMJ from excessive clenching and grinding, and longstanding occlusal force imbalances. This overuse typically results in spasms and pain/sensitivity in the muscles of mastication.
It was important to ensure that the orthotic was fabricated in a manner that stabilized the jaw position to a healthy placement to minimize muscle activity and the patient’s pain and symptoms. The patient was taught therapeutic exercises by the dental team. These exercises first were done in-office, and then continued by the patient at home. The importance of continuing the regimen at home was emphasized to the patient. If treatment did not continue after the patient left the office, she would not progress in her care. By purchasing—and correctly and regularly using—the home care kit, including the Alpha Stim AID, the patient learned and benefited from the proper preventative measures and methods to stabilize and maintain her jaw health.
Treatment Outcome
The patient underwent in-office therapeutic rehabilitation as previously described for 6 weeks. In addition to fabricating a custom rehabilitation orthotic for the mouth, 3 sequential occlusal equilibrations, or bite adjustments, were performed to correct bite imbalances.
At 6 weeks, the patient’s health and stability were confirmed with a digital ROM test. Range of motion values were found to be equal to or above physiologic norms (Figures 4 and 5). Dental bite force balance also was confirmed with the T-Scan analysis, which revealed left/right balance at 52%/48%, well within physiologic norms and tooth force readings at normal levels (Figure 6).
Conclusion
Dentists can create a pathway of care that offers predictable, reliable, and long-lasting relief from pain and restored function to patients suffering from the symptoms of DMSD. These include chronic headaches and force related dental conditions. Using a systematic approach to assessing and treating these conditions that incorporates technologies used for years in sports medicine (TruDenta), they can confidently provide much needed care to individuals who haven’t yet found the relief they’ve been seeking. Additionally, as in the case presented here, restoring balance, function, and overall well-being to the lives of longsuffering patients provides dentists and their teams with pride and professional satisfaction.
About the Author
Dr. Harrell is a practicing dentist in Charlotte, NC. His practice focuses on treating advanced restorative and TMD cases with the latest digital technologies. He has also pioneered the concept of the dental-based headache center for treatment of patients with chronic headaches, TMD, and facial pain. He can be reached at drrobharrell@charlotteheadachecenter.com. Disclosure: Dr. Harrell is a paid consultant for Dental Resource Systems, Inc.
References
- Junge D. Oral Sensorimotor Function. New Haven, MO: Medico Dental Media International; 1998.
- Okeson JP. Management of Temporomandibular Disorders and Occlusion. 6th ed. St. Louis, MO: Mosby Elsevier; 2008.
- National Headache Foundation. Migraine. headaches.org/education/Headache_Topic_She ets/Migraine. Accessed July 10, 2013.
- Sessle BJ. Mechanisms of oral somatosensory and motor functions and their clinical correlates. J Oral Rehabil. 2006;33:243-261.
- US News and World Report. Headache. 2006. health.usnews.com/health-conditions/brainhealth/ headache. Accessed July 10, 2013.
- American Dental Association. Dentists: doctors of oral health. ada.org/4504.aspx. Accessed July 10, 2013.
- Kerstein RB. Reducing chronic masseter and temporalis muscular hyperactivity with computerguided occlusal adjustments. Compend Contin Educ Dent. 2010;31:530-538.
- Bogduk N. The neck and headaches. Neurol Clin. 2004;22:151-171, vii.
- Tysowsky GW. The science behind lithium disilicate: a metal-free alternative. Dent Today. 2009;28:112-113.
- Strub JR, Rekow ED, Witkowski S. Computeraided design and fabrication of dental restorations: current systems and future possibilities. J Am Dent Assoc. 2006;137:1289-1296.
- Kugel G. Materials continue to expand dentistry’s options. Compend Contin Educ Dent. 2012;33:80.
- Dawson PE. Functional Occlusion: From TMJ to Smile Design. St. Louis, MO: Mosby Elsevier; 2007.
- Ogince M, Hall T, Robinson K, et al. The diagnostic validity of the cervical flexion-rotation test in C1/2-related cervicogenic headache. Man Ther. 2007;12:256-262.
- Garg AK. Analyzing dental occlusion for implants: Tekscan’s TScan III. Dent Implantol Update. 2007;18:65-70.
- Koos B, Godt A, Schille C, et al. Precision of an instrumentation-based method of analyzing occlusion and its resulting distribution of forces in the dental arch. J Orofac Orthop. 2010;71:403-410.
- Koos B, Höller J, Schille C, et al. Time-dependent analysis and representation of force distribution and occlusion contact in the masticatory cycle. J Orofac Orthop. 2012;73:204-214.
- Francisconi LF, Graeff MS, Martins Lde M, et al. The effects of occlusal loading on the margins of cervical restorations. J Am Dent Assoc. 2009;140:1275-1282.
- Hess LA. The relevance of occlusion in the golden age of esthetics. Inside Dentistry. 2008;4:38- 44.
- McNeill C. Occlusion: what it is and what it is not. J Calif Dent Assoc. 2000;28:748-758.
- Mackie A, Lyons K. The role of occlusion in temporomandibular disorders—a review of the literature. N Z Dent J. 2008;104:54-59.
- Frisardi G, Chessa G, Sau G, et al. Trigeminal electrophysiology: a 2 x 2 matrix model for differential diagnosis between temporomandibular disorders and orofacial pain. BMC Musculoskelet Disord. 2010;11:141.
- Hegarty AM, Zakrzewska JM. Differential diagnosis for orofacial pain, including sinusitis, TMD, trigeminal neuralgia. Dent Update. 2011;38:396- 406.
- Kampe T. Function and dysfunction of the masticatory system in individuals with intact and restored dentitions. A clinical, psychological and physiological study. Swed Dent J Suppl. 1987;42:1-68.
- Lodetti G, Mapelli A, Musto F, et al. EMG spectral characteristics of masticatory muscles and upper trapezius during maximum voluntary teeth clenching. J Electromyogr Kinesiol. 2012;22:103- 109.
- Ohrbach R, Fillingim RB, Mulkey F, et al. Clinical findings and pain symptoms as potential risk factors for chronic TMD: descriptive data and empirically identified domains from the OPPERA casecontrol study. J Pain. 2011;12(suppl 11):T27- T45.
- Velly AM, Look JO, Carlson C, et al. The effect of catastrophizing and depression on chronic pain—a prospective cohort study of temporomandibular muscle and joint pain disorders. Pain. 2011;152:2377-2383.
- Ackerman JL, Ackerman MB, Kean MR. A Philadelphia fable: how ideal occlusion became the philosopher’s stone of orthodontics. Angle Orthod. 2007;77:192-194.
- Maness WL. Force movie. A time and force view of occlusion. Compend Contin Educ Dent. 1989;10:404-408.
- Kerstein RB. Treatment of myofascial pain dysfunction syndrome with occlusal therapy to reduce lengthy disclusion time—a recall evaluation. Cranio. 1995;13:105-115.
- Wright EF. Manual of Temporomandibular Disorders. 2nd ed. Ames, IA: Wiley-Blackwell; 2009.
- Didier H, Marchetti C, Borromeo G, et al. Chronic daily headache: suggestion for the neuromuscular oral therapy. Neurol Sci. 2011;32(suppl1):S161-S164.
- Cairns BE. Pathophysiology of TMD pain—basic mechanisms and their implications for pharmacotherapy. J Oral Rehabil. 2010;37:391-410.
- Glaros AG, Williams K, Lausten L. The role of parafunctions, emotions and stress in predicting facial pain. J Am Dent Assoc. 2005;136:451- 458.
- Fernández-de-las-Peñas C, Cuadrado ML, Arendt- Nielson L, et al. Myofascial trigger points and sensitization: an updated pain model for tension-type headache. Cephalalgia. 2007;27:383-393.
- Glaros AG. Temporomandibular disorders and facial pain: a psychophysiological perspective. Appl Psychophysiol Biofeedback. 2008;33:161- 171.
- Okeson JP, de Leeuw R. Differential diagnosis of temporomandibular disorders and other orofacial pain disorders. Dent Clin North Am. 2011;55:105-120.
- Cameron MH. Physical Agents in Rehabilitation: From Research to Practice. 3rd ed. St. Louis, MO: Saunders Elsevier; 2009.
- Öz S, Gökçen-Röhlig B, Saruhanoglu A, et al. Management of myofascial pain: low-level laser therapy versus occlusal splints. J Craniofac Surg. 2010;21:1722-1728.
- Marini I, Gatto MR, Bonetti GA. Effects of superpulsed low-level laser therapy on temporomandibular joint pain. Clin J Pain. 2010;26: 611- 616.
- Srbely JZ, Dickey JP. Randomized controlled study of the antinociceptive effect of ultrasound on trigger point sensitivity: novel applications in myofascial therapy? Clin Rehabil. 2007;21:411- 417.
- Aguilera FJ, Martín DP, Masanet RA, et al. Immediate effect of ultrasound and ischemic compression techniques for the treatment of trapezius latent myofascial trigger points in healthy subjects: a randomized controlled study. J Manipulative Physiol Ther. 2009;32:515-520.
- Zuim PR, Garcia AR, Turcio KH, et al. Evaluation of microcurrent electrical nerve stimulation (MENS) effectiveness on muscle pain in temporomandibular disorders patients. J Appl Oral Sci. 2006;14: 61-66.
- Morphett AL, Crawford CM, Lee D. The use of electromagnetic tracking technology for measurement of passive cervical range of motion: a pilot study. J Manipulative Physiol Ther. 2003;26:152-159.
- Kerstein RB. Combining technologies: a computerized occlusal analysis system synchronized with a computerized electromyography system. Cranio. 2004;22:96-109.
- Kerstein RB. Current applications of computerized occlusal analysis in dental medicine. Gen Dent. 2001;49:521-530. Supplemental Reading List DiMatteo AM, Montgomery MW. Understanding, Assessing & Treating Dentomandibular Sensorimotor Dysfunction. Fort Lauderdale, FL: Dental Resource Systems; 2012. Forssell H, Kirveskari P, Kangasniemi P. Effect of occlusal adjustment on mandibular dysfunction. A double-blind study. Acta Odontol Scand. 1986;44:63-69. Karppinen K, Eklund S, Suoninen E, et al. Adjustment of dental occlusion in treatment of chronic cervicobrachial pain and headache. J Oral Rehabil. 1999;26:715-721. Silverman MM. Headache from pathology-producing occlusion of the teeth. Headache. 1971;11:35-46.





 © 2025 - NATIONAL DENTAL SYSTEMS, INC. | 430 NORTH MAIN ST. SALEM, UT 84653 | CALL US TOLL-FREE 855-770-4002
© 2025 - NATIONAL DENTAL SYSTEMS, INC. | 430 NORTH MAIN ST. SALEM, UT 84653 | CALL US TOLL-FREE 855-770-4002